Attention all patients and visitors
Please contact your surgeon’s office prior to your surgical date if you:
- are experiencing any cold/ flu symptoms or,
- have tested positive for COVID-19
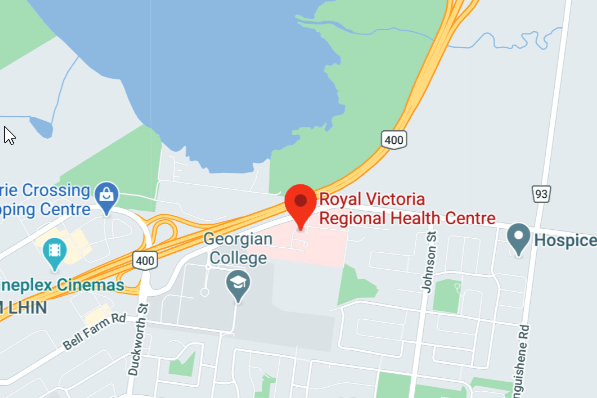
Directions
Pre Surgery Treatment Clinic Patients
On the day of your scheduled Pre Surgery Treatment Clinic appointment, please report to Central Registration at Atrium (Level 2). Please wash your hands with hand sanitizer and put on a hospital mask. Proceed to Kiosk to register for your appointment.
Day of Surgery Patients
On the day of surgery report directly to the Atrium Entrance level 2. Please wash your hands with hand sanitizer and put on a hospital mask. Proceed to Central Registration.
Contact Us
Managers
Phone: 705-728-9090
Laura Lloyd, Manager, Perianesthesia Services Ext. 46511
Jamie Bolton, Endoscopy, MDRD, Surgery Outpatient Clinics Ext. 46531
Kyla McKenzie, Operating Room, OR Bookings & Anesthetic Care Team Ext. 46510
Bonnie Berry, Inpatient Surgery 2 Ext. 46710
Yvonne Moloney, Inpatient Surgery 3 & Surgical Stepdown Unit Ext. 46810
Based on your health assesment by your physician 3 weeks prior to your surgery, you should have an appointment with the pre-surgery treatment clinic 7-10 days before your surgery.
Your appointment may last between 1-3 hours depending on your specific needs.
The Pre-Surgery Treatment Clinic provides pre-operative patient assessment, diagnostic testing and education in preparation for your surgery. Your appointment with the pre-surgery treatment clinic should be 7-10 days prior to your surgery date. The purpose of the appointment is to help ensure you are prepared for your upcoming surgery/procedure.
If your screening/assessment is over the phone, please have the anaesthetic questionnaire and the Pre-surgery medication review completed so the nurse can review this information with you.
If you have not already received these documents from the Surgeon’s office please print the PDFs above.
If in person screening appointment, please bring your surgery package provided by the surgeons office and have the anesthetic questionnaire and Pre-admission medication review completed. If you have not received the documents, please print, complete and bring them with you. In addition, please bring your medications and current pharmacy list with you and be prepared that the appointment may last between 1-3 hours, depending on your specific needs.
If you have not received the documents listed below from your Surgeon, please print and complete these documents and bring them on the day of your surgery. They must be completed prior to your arrival.
Contact Us
705-728-9090 Ext. 46740
Directions
From the Main Entrance follow the Main Blue Navigation Line to the Atruim (Orange) Elevators. Take elevator to Level 1 then turn left and follow the Blue Navigation Line to Pre-Surgery Treatment Clinic.
Hours of Operation
Monday – Friday 8:00 a.m. – 4:00 p.m.
If for any reason, you cannot keep your appointment, call your surgeon. If you must cancel the evening, night or weekend prior to surgery please notify the hospital at 705-728-9090 ext. 46505 and leave a message.
Contact Us
Patient Help Line: 705-728-9090 Ext. 46740
Directions
Central Registration is located on Level 2- Atrium Entrance across from Victoria’s Gift Shop.
Hours of Operation
Monday – Friday 6:00 a.m. – 4:00 p.m.
The Day Before Your Surgery
You will receive a call between 12:30 pm and 4:00 pm. Providing you with arrival time and instructions for your surgery. Please ensure you have provided your preferred phone number to the surgeon’s office and have someone to receive the call or that your voicemail clearly states your name to enable us to leave a detailed message. If your surgery is on a Monday, you will receive a call on the Friday prior.
The Day of Your Surgery
Please report to the Central/Surgical Registration area (located on Level 2) at your assigned time.
Please follow the specific instructions you have been provided with to prevent delay or cancellation of your surgery.
- Do not eat anything after midnight.
- Up until 1 hour before your arrival time you may drink clear fluids (water, clear tea or coffee with sugar only, apple juice, cranberry juice, sports drinks or kool aid)
- Cataract patients are required to wear a button-down shirt (you will not need to change into hospital attire)
- Unless instructed otherwise, take all of your usual morning oral medication with a sip of water at 6 am the day of your surgery
- Bring your Ontario health Card to the hospital with you
- Bath or shower at home prior to surgery
- Please arrive with all make-up removed. Do not wear perfume or aftershave
- Remove all body jewellery and leave valuables at home. There is no secure storage area.
- Please bring your reading glasses and glass case (if needed).
- Patients under the age of 16 must be accompanied by a parent or guardian to confirm consent for the surgery.
- Do not drink alcoholic beverages (including wine and beer) for at least 12 hours prior to your arrival for surgery.
- Do no use any recreational drugs such as marijuana for at least 12 hours prior to your surgery.
- Stop CBD oil 4 hours before surgery.
- Do not use cocaine, ecstasy, ect. For at least 48 hours prior to surgery.
- Wear comfortable loose fitting clothing and flat-soled shoes.
Special Instructions for Children
- Children are encouraged to bring a favourite toy
- Bottle-fed babies – please bring a bottle the baby is familiar with
If your child has a cough, fever or cold symptoms, please contact the surgeons office for instructions.
Additional instructions
If you are coming in for surgery and going home the same day:
After your surgical procedure you will not be permitted to drive yourself home, or leave the hospital unaccompanied in a taxi.
Arrangements must be made in advance to have someone accompany you home and remain with you overnight.
If you are coming in for surgery and are required to stay overnight:
Should you require items for an overnight stay please pack them in a small bag
Review the visiting instructions on the RVH main page
Stand-by/add-on surgery is subject to delay as a result of a life and death procedure to be completed first.
This is often an unexpected and sudden delay. We endeavor to keep you informed and as up to date as possible. There are times that your surgery may not be done on the scheduled dated and may require re-booking.
If scheduled for a standby/add on surgery on a weekday:
Surgical Services Staff will call you the evening prior to your surgery and provide instructions.
You will receive another call the morning of your surgery confirming instructions and providing an arrival time
If scheduled for standby/add on procedures on a weekend or holiday:
Surgical Services Staff will contact you the evening prior to your surgery with specific instructions and arrival times for your surgery
All patients undergoing hip or knee replacement surgery will be asked to complete PROMs before and after their surgery. You will be ask to provide information on your health status and quality of life. Completion of the PROMs survey is voluntary.
When do I complete PROMs?
- During your pre-op assessment visit before your surgery
- 3 months after your surgery
- 12 months after your surgery
Why are patients being asked to complete PROMs?
- Provide insight into the effectiveness of care from the patient perspective
- Gather valuable data across Ontario to improve patient care
Musculoskeletal Central Intake Form
Colposcopy Program Central Intake Referral Form
The Acute Pain Service is a multidisciplinary team comprised of anesthesiologist, anesthesia assistants trained in acute pain management, in-patient nurses and pharmacists. The goal of the Acute Pain Service is to assist patients through their surgical recovery by minimizing pain and reducing post-operative complications.
The type of pain management employed is determined by a number of factors, including type of surgery, type of anesthetic and most importantly, specific patient’s needs. The specific therapies employed to manage pain may include: oral medication, intravenous self-controlled pain pumps, regional anesthetic blocks or epidural infusions. The Acute Pain Service team will work with each patient to develop the best strategy to optimize their post-operative recovery with your surgeon and other health care providers.
Post-operative Pain Management Education for Patients
The management of post-operative pain begins at home with the development of reasonable expectations and goals for pain relief. Although absolute avoidance of pain following surgery would be ideal, the reality is that some discomfort is likely unavoidable. However, with the use “multi-modal” (medications from different classifications) therapy and non-pharmacologic techniques, the Acute Pain Service will ensure that our patients have level of pain that is manageable and allows for a safer and quicker recovery.
Each patient within the Acute Pain Service will have the opportunity to discuss their individualized pain management plan with a dedicated anesthesiologist or anesthesia assistant in their pre-surgery appointment or the day of surgery. Part of that discussion will include the type of anesthetic utilized, such as spinal, neuraxial anesthesia, general anesthesia, regional anesthesia or epidural anesthesia/analgesia.
Immediately prior to surgery, Acute Pain Service patients will be provided with several oral medications. This “multi-modal” therapy will be continued throughout the perioperative period and works to minimize narcotic (opioid) use.
Advantages of Multi-Modal Pain Management include:
- Reduces the dependency on narcotic (opioid) drugs to achieve adequate pain management
- Reduces the overall side effects of the medications (i.e., drowsiness, nausea)
- Allows patients to feel more alert following surgery
- Allows for earlier ambulation
- Allow for earlier progression of diet (i.e., clear fluids to full diet)
- Allows for earlier return of normal bowel and bladder function
- Decreased incidence of confusion post-operatively
- Earlier recovery and discharge home
Although each patient’s medications will be tailored to their particular surgery, anesthetic and pre-existing medical condition(s), patients will be provided with around the clock medications for a number of classifications (multi-modal) including: anti-inflammatories, acetaminophen, long acting capsules and stronger tablets used for “breakthrough” pain. “Breakthrough” pain is pain that is not effectively managed with scheduled medications alone. Typically this type of pain may be associated with an increase in activity, such as physiotherapy or ambulation. Patients are encouraged to speak with their nursing staff and take additional medications as needed to promote optimum comfort. By providing these medications around the clock, pain is managed and side effects are minimized. Although it may seem strange to have nursing staff wake patients to take medications, the regular dosing has been proven to be more effective and well tolerated.
Medications provided by intravenous or epidural routes are often used in conjunction with oral tablets to provide additional analgesia for patients requiring them. Patient Controlled Analgesia pumps and Patient Controlled Epidural Analgesia pumps are an option that allow the patient to push a button that is attached to the intravenous line or epidural, which then delivers a small effective dose of medication. These devices have multiple pre-set, safe limits and are used exclusively by the patient. Nursing staff and family are not allowed to touch the pump control button. Patient Controlled Epidural Analgesia is a method often used for patients undergoing large abdominal, urologic or vascular surgeries, as well as for mothers in the birthing unit. The anesthesiologist, anesthesia assistant and nursing staff will provide additional education for patients with these systems to ensure that patients understand how to effectively use them.
There are also a number of other pain management techniques to improve patient comfort. These can include application of cold or heat packs, relaxation techniques, distraction (television, music and games) or activities that patients find relaxing and therapeutic.
Assessing Your Pain
Pain is not easy to measure. Each patient room is equipped with a “white board” that your nurse will explain on arrival to the area. There are a number of “faces” at the bottom of the board, which help in assigning a numeric value or pain score (0-10) to your discomfort. Your pain score will help the nursing staff determine the most effective medications to administer to improve your comfort. These pain scores will also be used by the Acute Pain Service team to evaluate how effective any changes to your multi-modal therapy have been. Staff will be asking you with each visit how comfortable you are and how effective your pain medications are. It is important that patients communicate with the nursing staff to ensure that comfort is achieved.
Nursing staff will also be focusing on the type of pain that patients are experiencing and may ask questions about the “quality” of the pain. Is it burning, sharp, throbbing, and aching? Where is the pain? Does it travel to other parts of your body? Is there a certain position that makes you feel better or worse? How effective are the pain medications when you take them? All of these questions will assist the nursing staff to effectively manage your post-operative pain.
Patients are encouraged to speak to the anesthesiologist, the anesthesia assistant and nursing staff about any questions related to their pain and treatment while at RVH.
References
RVH – Information for Patients Having Surgery – Spinal / Epidural Anesthesia
RVH – Information for Patients Having Surgery – Regional Anesthesia, Upper and Lower Extremities
RVH – Pain Management – Patient Controlled Analgesia
RVH Department of Anesthesia
Pasero, C., McCaffrey, M. Pain Assessment and Pharmacologic Management. Mosby. St. Louis. (2011)
The Department of Anesthesia provide Anesthesia care for patients undergoing surgical procedures and carefully assess patients preoperatively and educate them about their surgeries
The Department also runs a comprehensive Acute Pain Service to ensure that patients have appropriate pain management during their post-operative stay. The care of postoperative pain also includes regional anesthesia (Nerve Blocks for acute pain) where an anesthesiologist, using ultrasound guidance, delivers local anesthetic close to a nerve to provide hours of relief after certain surgeries.
Anesthesiologists play an important role in the birthing unit, providing pain control during labour and surgical anesthesia during caesarean sections.
They also provide relief for patients with chronic spinal pain through Fluoroscopy (X-Ray) guided and Ultrasound guided nerve block and epidural injections.
You may also encounter anesthesiologists caring for patients in areas like the Imaging Department, Emergency Room, Cardiac Care Unit (CCU) and Intensive Care Unit (ICU).
Currently, there are 24 dedicated anesthesiologists on staff at the hospital providing 24 hour coverage for both elective and emergency care throughout the hospital. You may also encounter our excellent anesthesia assistants who work under the supervision of the physicians to provide high quality care for our patients.
Musculoskeletal Central Intake / Musculoskeletal Rapid Access Clinic
The North Simcoe Muskoka LHIN (region) has introduced the Musculoskeletal (MSK) Central Intake and Rapid Access Clinics (RAC) as part of a provincial initiative to improve timely access to quality care.
Rapid Access Clinics locations:
- Collingwood General and Marine Hospital
- Orillia Soldiers’ Memorial Hospital
•Royal Victoria Regional Health Centre
Contact Us
Phone: 705-728-9090 Ext. 46950
Fax: 705-792-3329
Toll Free Fax: 1-866-449-0994
The MSK Central Intake acts as one point of contact for all referrals related to hip and knee arthritis across the region. Patients will be assessed by an Advanced Practice Physiotherapist (APP) at one of three RACs in our region. Patients deemed ready for surgery will then go on to see the orthopaedic surgeon.
What to Bring to Your Appointment:
· Health Card and/or applicable insurance (ie WSIB, etc)
· X-rays or Diagnostic Imaging Films or CDs
· Please wear/bring loose fitting clothes for the joint being assessed
· Medication list
The APP is a specially trained physiotherapist that works collaboratively with the orthopaedic surgeons. This model focuses on providing quicker access for patients while maintaining thorough patient education and treatment recommendations. This streamlined process has improved access and quality of care for patients with hip and knee arthritis including reduced wait times for both assessment and surgery.
Prior to referral, primary care practitioners should discuss with their patients if they would prefer their assessment to take place at the location closest to their home, or if they would prefer to attend the first available assessment within the LHIN (region).
Joint Assessment Referral Process
All patients require a referral from a referring practitioner.
Referral Forms that are not complete will be returned to the referring practitioner and a new referral will be required. Complete referrals facilitate having patients seen in a timely manner and allows accurate provincial wait times to be captured for our LHIN (region).
Once a patient has been booked for a consultation appointment at the clinic, they are contacted directly and/or by their referring practitioner with appointment information and any specific instructions required (paperwork and x-ray requirements).
Fax:
Referring practitioner can fax the completed referral form with an attached x-ray report (within the past 6 months) to 705-792-3329
Equipped with the latest technology, our three room endoscopy suites and one room cystoscopy (OR 11) suite provides a comprehensive range of diagnostic and therapeutic procedures on a scheduled or emergency basis. After hours, the Surgical Suite provides coverage.
Referral Instructions
The Surgeon/Specialist offices book procedures directly with the OR scheduling Staff.
RVH Endoscopy Patient Survey
If you have been a recent RVH Endoscopy patient, the Endoscopy Department kindly requests that you complete this short survey to help us improve the patient experience.
RVH has approximately 75 inpatient beds targeted to provide care for pre and post-operative patients. These beds are located on two inpatient units: Surgery 2 and Surgery 3. Our surgical services include: general surgery, plastics, ENT, ophthalmology, urology, orthopedics, dental, maxillofacial, vascular, gynecology, and gyneoncology services.
A patient care manager is available to address your needs or concerns
Monday – Friday 8:00 am – 4:00 pm.The units all have nurse leaders referred to as the Resource Nurse also available to address your needs and concerns
7 days a week 7:00 am – 7:00 pm.
Contact Us
Surgery 2: 705-728-9090 Ext. 46888
Surgery 3: 705-728-9090 Ext. 46440
The 2 units will specialize in servicing your individual surgical needs. Surgery 2 service is specialized in optimizing high quality orthopedic outcomes. Surgery 3 has a specialized service meeting the demands of a more acute population in our Surgical Step-down Unit (SSDU) and our vascular, ENT, gynecology and gyneoncology patients.
The inpatient surgical units utilize a team approach to provide all aspects of your care and will keep you and your family informed of all care decisions.
(MDRD) is a 24 hour, 7 days a week support service responsible for cleaning, decontamination, inspection, assembly, packaging, and sterilization of medical devices/equipment. The department is centrally located in RVH on the first floor. MDRD has recently centralized reprocessing and added a new area for reprocessing flexible endoscopes of all kinds.
MDRD staff is comprised of Medical Device Reprocessing Technicians (MDRT) who have completed the Medical Device Reprocessing course or a Medical Device Reprocessing Program at a Community College.
MDRD is responsible for sterilizing thousands of instruments and instrument sets every year which are needed to perform surgeries and procedures throughout the health centre. To achieve this MDRD follows the Canadian Standards Association and Provincial Infectious Disease Advisory Committee (PIDAC), and Best Practices for Cleaning Disinfection and Sterilization of Medical Equipment/Devices guidelines. There are many quality assurance checks medical devices/equipment undergo before being used in procedures. MDRT’s pick equipment and supplies for patient surgeries for the operating rooms. They also assist the operating rooms daily with any equipment needs. Our team ensures the Physicians and Nurses have everything they need for surgical procedures and out-patient clinics.
Following your surgery you will recover in the Post Anesthetic Care Unit (Phase 1). Registered Nurses with specialized training will monitor you closely to ensure that you recover safely and comfortably. While each person and circumstance is different, this on average takes approximately one hour.
Once you are awake and comfortable, you will be transferred to your room where your Post Anesthetic Care Unit nurse will give a full report to your surgical nurse. You will be present for the report and invited to participate in your transfer of care.
If you are going home after your surgery, you will be transferred to Surgery Recovery (Phase 2) where our team of Registered Nurses and Registered Practical Nurses will complete your care.
In phase 2, depending on your surgical procedure, you will be transferred from your stretcher to a reclining lounge chair. This will encourage early ambulating (walking), promote deep breathing and optimal circulation. Your family member will be contacted regarding a pick up time by the surgery recovery nurse. The nurse will review the discharge instructions and prescription(s) (if provided), to the designated responsible adult.
If the patient is a child, only one parent will be able to accompany them.
You will be provided with written and verbal instructions specific to you and your surgical procedure and you will be given the opportunity to discuss any questions or concerns that you may have. You will also be provided with follow up care instructions and a prescription if required. This takes approximately 30 minutes depending on your procedure. Patients requiring Tonsillectomies will be required to stay for a total of 4 hours after their procedure and patients with Malignant Hyperthermia History will be required to stay for a total of 2.5 hours after their procedure.
Sometimes your surgeon will ask that you stay a little longer as he would like to see you before you go home. You may be asked to wait in the Surgery Recovery waiting area.
For your safety, your family member or friend will be required to drive you home and stay with you overnight.
You may receive a post- operative follow up phone call the day after your surgery to ensure a continuing, safe, comfortable recovery.
Hours of Operation
Monday – Thursday 8:00 a.m. – 3:00 p.m.
Friday 8:30 a.m. – 3:00 p.m.
Contact
Appointments are booked through the surgeon’s office. Please contact the surgeon’s office if you have any questions regarding your appointment.
Services Available Include:
- Cystoscopy Clinic
- Ear Nose and Throat Clinic
- General Surgery Clinic
- Gynecology Clinic
- Hand Therapy Clinic
- Ophthalmology Clinic
- Orthopedic Clinic
- Pain Management Clinic
- Plastic Surgery Clinic
- Urology Clinic
- Vascular Clinic
Eleven modern, fully-equipped Operating Rooms are available for elective and urgent surgical procedures. Our highly qualified team of Anesthesiologists, Nurses, Surgeons, other health care professionals and support staff provide a diverse range of surgical procedures on a scheduled or emergency basis.
Surgical Specialties
- General Surgery
- Vascular Surgery
- Orthopedic Surgery
- Plastic Surgery
- Ophthalmology Surgery
- Ear, Nose and Throat Surgery
- Dental and Oral Surgery
- Maxillofacial Surgery
- Urology Surgery
- Gynecology Oncology
- Gynecology Surgery
- Cystoscopy
Surgical Safety Checklist
On the day of your procedure, you will be asked to participate in the Surgical Safety Checklist with the members of the surgical team. This process will be carried out prior to your procedure and will occur again during and at the end of your procedure.
Ears, Nose and Throat Surgery/Respiratory Surgery
General Information
General Surgery
Gynecology Surgery
Maxillofacial Surgery/Orthognathic Surgery
Orthopaedic Surgery
Pain Management
Interventional Pain Clinic
Plastic Surgery
Urology Surgery
Vascular Surgeries
Screening
Musculoskeletal Central Intake / Musculoskeletal Rapid Access Clinic
Directions
Central Registration is located on Level 2 in the Atrium Entrance across from Victoria’s Gift Shop
Inpatient Surgical Services
Directions
From the Main Entrance follow the Blue Navigation Line to the Central (Green) Elevator. Take it to Level 4
Surgery Treatment Clinic (STC)
From Level 2 take the Atrium (Orange) Elevator to Level 1. Turn left out of the elevator and follow the Blue Navigation Line to proceed to the Surgery Treatment Clinic.