Manager: Jennifer Kluszczynski
Phone: 705-728-9090 Ext. 47610
Unit phone extension: 705-728-9090 Ext. 47620
The ICU is a 15-bed specialized closed unit designed to care for patients who are critically ill or injured and whose condition is requires comprehensive critical care and constant monitoring.
Our ICU has state-of-the-art equipment and specially trained staff to meet the complex needs of the critically ill patients.
Associated with our ICU is a Critical Care Outreach Team (CCOT). The CCOT team is led by an Intensivist and includes specially trained registered nurses and respiratory therapists.
- CCOT brings critical care through the health center 24/7.
- CCOT follows up with all patients transferred out of the ICU for a minimum of 48 hours to assist in the transition and safety of the patient.
- CCOT works in partnership with teams on inpatients wards and with critical care to identify, assess and respond to the needs of seriously ill patients; providing a consultation service.
Lift the phone in the waiting room to enter.
A comprehensive team of Health Professionals and Support Staff work collaboratively to ensure that the best possible care is provided. The team consists of:
- Medical Director and Chief of Critical Care
- Operations Director of Critical Care
- Manager
- Intensivists
- Registered Nurses: RN
- Physician assistant: PA
- Clerical staff
- Respiratory Therapists: RT
- Dietitians
- Pharmacists
- Physiotherapists: PT
- Social Workers
- Support Staff (such as speech language pathologist, OT, Logistics, EVS)
- Volunteers
- Spiritual Care
- Many other members of team RVH who we call upon to assist with their specialty and contribution to critical care
Every critical care patient is a unique individual. We admit many patients to critical care with the same diagnosis, yet each patient will have a different overall response and experience. A patient’s age, prior state of health or the presence of other medical conditions will influence their progress. We need to know as much as possible about our patient’s health and medication history so that we can customize their medical plan.
As soon as your family member is admitted to RVH, you will be asked about their past medical history and whether they have any allergies. This information is very important to our team so that we don’t miss anything important. You will also be asked for a current list of medications.
Medication Reconciliation is completed by a pharmacist and is a detailed review of all the patient’s medications.
In addition to knowing the medications that have been ordered for your family member, we need to know if your family member has been taking the medication recently. If you don’t know your family member’s current medication list, it will help us to know the name of your family member’s pharmacy (or pharmacies) and their family doctor. This information will help us to check to see if any of your family member’s symptoms could be related to their medications, or if there are any medications that need to be continued when they are critically ill. Your family member’s pharmacy and family doctor should also have their allergy information.
It also helps the healthcare team to know how your family member usually copes with stress. If they had difficulty before their admission, they may need extra help during their recovery. For example, knowing any strategies that your family member uses to manage symptoms of anxiety or depression may be helpful when planning your family member’s care. Patients who regularly use recreational drugs, alcohol and tobacco may experience withdrawal symptoms that we may need to manage. If you have information that might help us to care for your family member, please let your family member’s nurse and care team know.
There are some things that are part of every patient’s daily ICU routine.
Interprofessional Rounds
Start at 0930 daily and involve the entire interprofessional team led by the Intensivist and include the primary nurse, the resource nurse, the respiratory therapist, physiotherapist, pharmacist, dietitian and physician assistant. At these rounds the nurse provides an overall review of the patient and then each member contributes their clinical expertise.
During rounds
We examine the patient’s medical problems, treatment plan and response to treatments. We incorporate the expertise of the many different healthcare professionals to determine the best possible treatment plan for each individual patient.
We share our plans openly with our patients and their substitute decision-makers. We encourage family to ask questions about the plan or any aspect of your family member’s care. Families are an important part of the team and we value your input.
Comfort Measures
- Bathing, skincare, repositioning and linen changes are all examples of routine strategies to help make patients more comfortable.
- Patients are repositioned frequently and skin is inspected to monitor for any signs of skin breakdown. Critically ill patients have many reasons for skin problems, including immobility, low blood flow to the tissue, use of drugs that decrease blood flow to the skin, poor nutrition, edema, moisture (sweating, draining wounds or incontinence), surgery or trauma, rashes, medication and infection.
- Patients with breathing tubes will experience a dry mouth. Although they cannot drink when a breathing tube is in place, their lips can be moistened with lubricants and their mouth rinsed with moist sponges. We can show the family how they can help with this for their loved one.
- Suctioning is a procedure that is done to help keep a patient’s airway open and free of mucous. Mucous is also called “secretions”. When a patient has a breathing tube in place, he or she will require intermittent suctioning. The frequency will depend on the quantity and thickness of the secretions.
- Family can help by holding the patients hand, talking in a comforting voice or reading favorite stories as this can provide familiarity and reduce anxiety for the patient.
- We encourage family to bring a picture of their loved one prior to their injury or illness. This helps us all see our patient as a person beyond their illness.
- Rest periods are an important part of the recovery process. The critical care patient needs rest to recover and often stimulation can cause stress to the patient. Speaking in soft calm tones and allowing the patient to sleep is important. Our patients can often get their days and nights confused, we make every effort to reduce night time stimulation.
Exercise
Critical care patients are at high risk for deconditioning. With the help of our excellent physiotherapist and equipment we work with our patients and push them to the best of their ability. After a critical illness even the simple tasks can be a challenge and we celebrate milestones throughout our patient’s journey.
During COVID we have had to alter our visiting practices at RVH and in our ICU. Please speak with your family member’s nurse to discuss the visiting.
We have adopted different ways to help you stay connected with your loved one. We can set up facetime with family and our patient, even if your loved one is not able to communicate with you this would enable you to be able to see and speak to them. We are able to use OTN – or a computer app to have you included in our interprofessional rounds. This would involve setting up an appointment via e mail the day prior, our clerk would able to assist you with this.
To protect the privacy and safety of all our patients and visitors, we ask that visitors check with the unit clerk, volunteer or nurse before each visit as you enter the unit.
When you visit for the first time, you will be instructed on how to perform hand hygiene and put on any required personal protective equipment. If you are the patient’s Substitute Decision-Maker (SDM), the nurse will tell you about the patient’s condition and orient you to the patient care area, equipment and sounds that you will see and hear. It can feel overwhelming and emotional the first few times you visit; our team understands. Please know that we are here to help support you and your family.
Critically ill patients are often unable to speak for themselves and we need to identify a Substitute Decision Maker. The selection of a Substitute Decision Maker is guided by the Health Care Consent Act and is appointed according to the following hierarchy:
- Power of Attorney
- Spouse (living together in a married or common-law relationship)
- Parent or child
- Siblings
- Other relatives
- Anyone can appoint an individual to act as a Substitute Decision Maker, prior to a need arising. A person appointed to make decisions about health care is called an “attorney for personal care”. This appointment can be written into a legal document, called a “Power of Attorney”. The person given Power of Attorney for personal care may be different than the person given Power of Attorney for financial issues. The appointment needs to be made when an individual is competent and capable of making this decision. Critically ill patients are often too ill or under the influence of medications that limit their ability to make informed decisions.
- A Substitute Decision Maker must be willing, available and capable of taking on this responsibility. If the individual identified does not meet this criteria, we move down the list to identify the most appropriate Substitute Decision Maker. If a patient does not have a Power of Attorney for Personal Care or an appropriate family member, a guardian can be appointed by the court.
- We have a social worker who can help you to identify the Substitute Decision Maker.
- It is important to remember that the SDM is the voice of the patient and they need to make decisions based upon what the patient would want.
- All patients admitted to RVH are asked about their wishes regarding life-support. When a patient is unable to tell us their wishes, we must rely on the Substitute Decision Maker to communicate the patient’s goals, wishes and beliefs.
- The success of any treatment depends upon a number of factors, such as the underlying reason for the emergency and the patients previous state of health. Life support and CPR do not cure the underlying health problem. These therapies may provide time for treatments to work. If the treatment fails, or there is no treatment for the patient’s disease, life support or emergency treatments may not benefit the patient.
- Every patient has the right to have their wishes regarding life-support discussed. It is our obligation to provide you with the information you need to make the best decision. Decisions can also be changed as the patient’s situation changes. Please talk to us about your family member’s wishes. If you would like more information about life-support decisions, please speak to a member of the health care team.
- If, after carefully reviewing the patient’s medical condition and progress, the family and medical team agree that further treatment is not in the patient’s best interest, a plan to withhold or withdraw life-support may be made. The plan will be individualized according to the wishes of the patient and family. The patient’s comfort is always a priority, regardless of the treatment plan.
As an important member of our team you need to remember to look after yourself.
- Rest and nutrition is a must.
- Try to take a few moments each day just for you; even a short walk can make a difference.
- You will be given a lot of information daily. You may find it helpful to start a journal to keep track of information and milestones of your loved one.
- Critical illness is a journey; there will be progress and set backs. This is expected. Your loved one needs you for the duration which is why taking the time to care for yourself is so important.
Critical Care Glossary
Arthritis Society
Canadian Cancer Society
Hearth & Stroke Foundation of Canada
Healthy Ontario
Cardiac Care Network of Ontario
Simcoe Country District Health Unit
World Health Organization
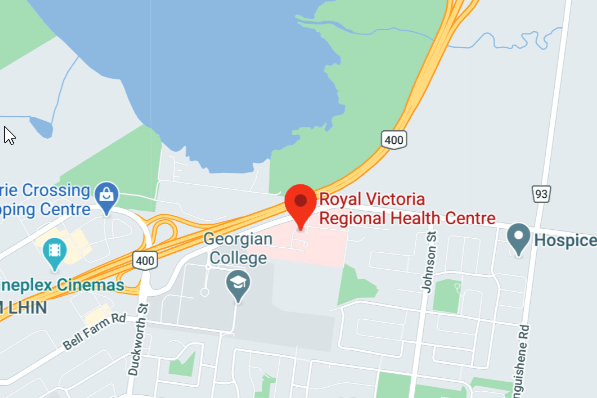
Step-by-step Directions
Street: Gallie Court
Travelling on Georgian Drive you will pass Georgian College and TURN RIGHT into the third entrance at Gallie Court. After the stop sign, proceed FORWARD and TURN RIGHT into RVH’s Main road entrance.
- You will see Rotary Place and RVH entrance signage
Parking: Main
Proceed FORWARD through RVH’s Main road entrance. RVH’s Main Parking lot can be found ON YOUR RIGHT.
- You will see Rotary Place on your right followed by parking gates
Entrance: Main
Enter RVH’s Main building entrance and FOLLOW the Blue Navigation Line TOWARDS the Atrium (Orange) Entrance.
- You will pass RVH’s Corridor Gallery
- You will pass the Central (Green) and Atrium (Orange) elevators
- You will pass Victoria’s Gift Shop on your right
Department: ICU
When you reach Central Registration, TURN LEFT walking through the double doors down the hallway.
TURN LEFT when you see hallway signage listing ICU.
Passing Endoscopy Recovery on your left, The ICU is ON YOUR RIGHT.